Mistakes in IBD – 13 mistakes, Ulcerative Colitis and Crohn’s patients do

1.Not understanding disease course in general: You should ask your doctor about how the disease behaves in general in patients? How much is the risk of relapses and complications?
2. Adherence to medicines: Many patients skip or stop medicines when they are symptom-free. Also, they stop the medicine if desired results are not seen. This is among most common mistake as this not only jeopardise patient for relapse but also is a risk of malnutrition. If they don’t get better, they should visit a doctor and the doctor can start other medicines. Step up approach of medicines is a well-established way for nonresponders.
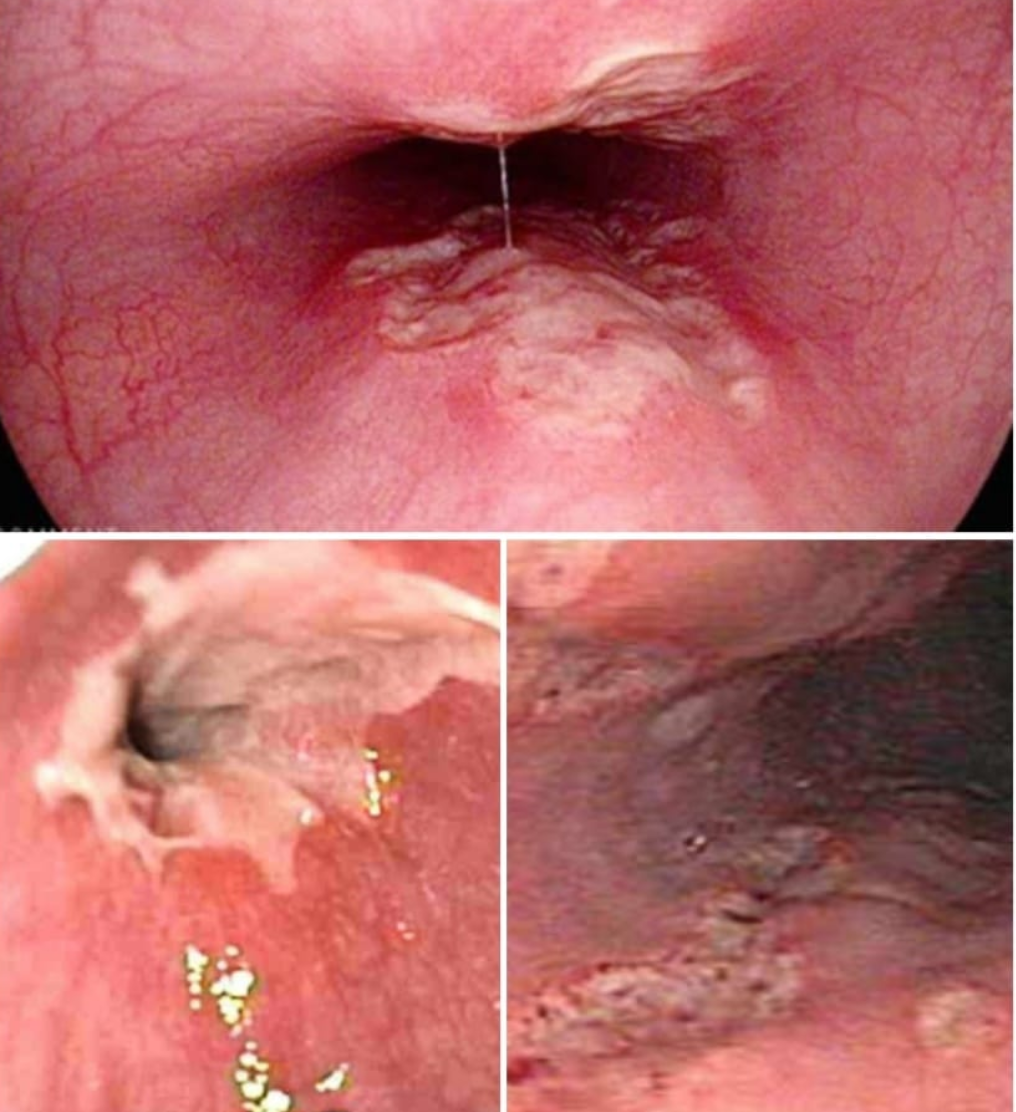
3.Not doing tests at certain intervals: Ulcerative colitis and Crohn’s disease patients need to do certain simple tests at a few months intervals. They also need to get endoscopies done at intervals. In IBD, absence of symptoms does not mean an absence of disease. In fact, many times there are no or minor symptoms but the disease progresses inside. Many patients are shocked when they diagnose with stricture on one bad day even with good compliance with medicines. What’s common in these patients is they didn’t go to a doctor for regular check-ups.
4.Not proper understanding of side effects: Ask your doctor about the side effects of medicines. Like Azathioprine can cause low Haemoglobin/white cells/platelets and liver inflammation. Biological medicines can have infusion reactions and increased risks for infections.
5.Starting Alternative medicines and stopping allopathy: Many patients have a gut feeling that allopathy medicines are harmful and other pathy medicines are free of side effects, which is not true. They stop Med and turn towards other pathies or even to quacks or some diet programs. Believe me, everyone eventually lands up with flare.
6.Diet restrictions: Some people omit food items from diet. There is no need for diet restrictions in quality and quantity. Some food better is avoided during flares only. This will predispose you to malnutrition and there will always be a feeling of illness even if you are symptom-free.
7.No bleeding/Diarrhoea equals Normalcy: Symptom-free does not mean disease-free. The disease remains in the body at low intensity. It takes months and years for complete mucosal healing. therefore, don’t stop the medicine and do regular follow-ups.
8.Misconceptions about Cure vs Control: Many patients don’t have a clear idea about this disease will get cured or they have to take medicines lifelong. For most patients, depending on symptoms, blood and endoscopy reports doctor tapers medicine to a minimum. In few patients, if mucosal healing is complete then the doctor can plan a medication-free trial with close follow-up.
9.Postponing doctor visit even if symptoms relapse: IBD patients have a good tolerance for symptoms and they wait for spontaneous recovery or take over-the-counter medicines and don’t do doctor visit early in relapse. This makes the disease more severe and recovery slow.
10.Taking a certain groups of pain killers: for any pain, IBD patients should not take NSAID group painkillers as they are known to exacerbate the disease.
11.Inadequate care when traveling about food/Water: Clean food and water are a must as food poisonings and intestinal infections aggravate the silent disease.
12.Addictions: Smoking cannot be tolerated as it can aggravates symptoms.
13.Stress management: Stressful events come to all of us but if you are not able to manage stress properly then it can aggravate the symptoms. Some patients need counseling and even treatment